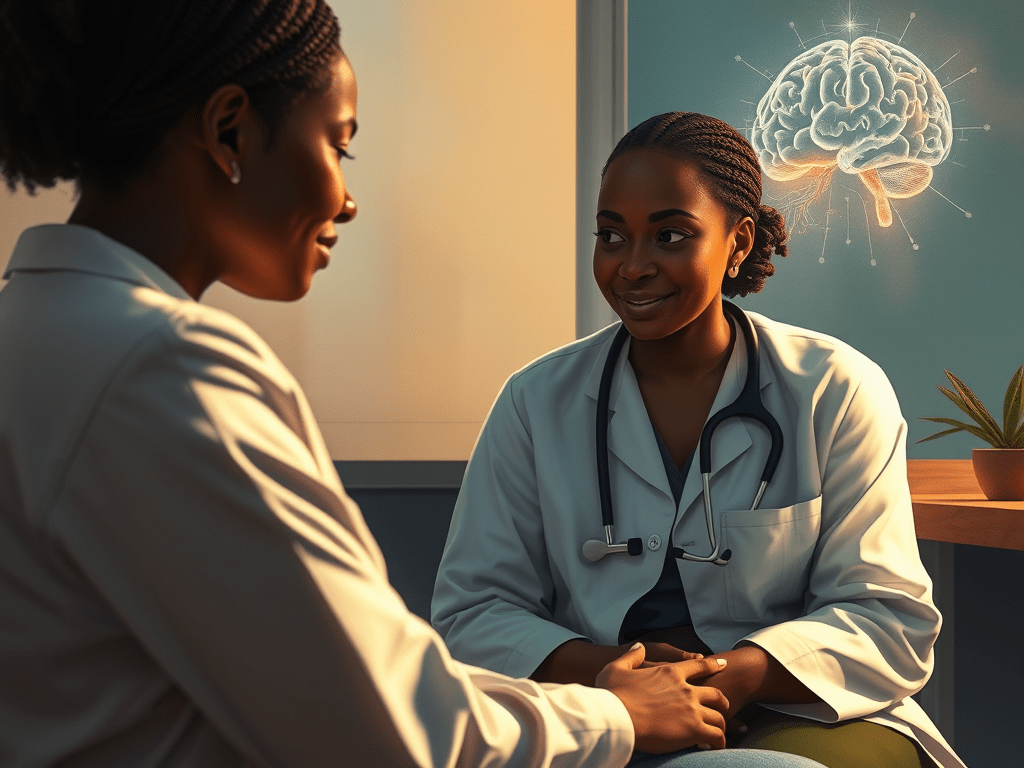
In the soft light of a Nairobi clinic, Dr. Aisha Mwangi listens as Fatuma, a young mother, describes the relentless fog that has settled over her mind since giving birth. “It’s like my brain forgot how to feel joy,” she says, voice breaking. Dr. Mwangi leans forward, gently: “Your brain didn’t forget — it’s just rewired in this season. But it can rewire again. That’s neuroplasticity, and it’s on your side.”
For too long in Fatuma’s community — and many like it — postpartum depression is mischaracterized as a weakness, a spiritual failing, or a passing mood. But modern neuroscience tells a radically different story: the brain is not fixed. It’s dynamic, capable of change. And that change can be guided.
The Science Behind How The Brain Rewire Itself
Neuroplasticity refers to the brain’s capacity to reorganize itself by forming new neural connections over time. These changes don’t just happen in childhood; they continue throughout our lives. Neuroscientific studies show that interventions like therapy, exercise, and meditation can lead to real biological change in the brain.
One systematic review found that meditation and mindfulness actually lead to structural and functional transformations in the brain — including increased cortical thickness in the prefrontal cortex and changes in connectivity.
Another meta-analysis of controlled trials reported that mindfulness-based interventions (MBIs) significantly boost peripheral levels of BDNF (brain-derived neurotrophic factor), a protein critical for neuroplasticity.https://pubmed.ncbi.nlm.nih.gov/33041891/
Moreover, in a 9-month randomized clinical trial, sustained contemplative training (meditation and mindfulness) not only increased BDNF but was also associated with reduced cortisol (a stress hormone) and increased volume in the hippocampal dentate gyrus — a region implicated in memory and emotional regulation.
These are not abstract lab findings. They show that consistent, intentional mental practices can reshape brain biology in ways that support resilience, emotional regulation, and healing.
Kenya’s Mental-Health Landscape: What The Data Actually Shows
In Kenya, the mental health burden is real — and the system is stretched. The Kenya Mental Health Action Plan 2021–2025, published by the Ministry of Health, explicitly calls for the expansion of community-level mental health care, training of community health volunteers in mental health, and the development of peer support networks.
Despite these policy goals, access remains limited: a recent national news report noted that more than 75% of Kenyans cannot access mental health services.https://www.the-star.co.ke/news/2022-04-20-95-of-kenyans-cant-access-mental-health-services-lobbies
Implementation research in Kenya also highlights how non-specialist health workers — such as community health workers without formal psychiatric training — can deliver effective mental health treatments (for depression and PTSD) through task-shifting. But scaling these models sustainably requires navigating policy, training, and funding barriers.
Turning Neuroscience Into Real-World Solutions
Here’s how neuroplasticity concepts can translate into accessible, science-based practices — especially in a Kenyan context.
- Mindfulness & Meditation
Why it helps: Regular practice rewires brain regions tied to emotion and self-regulation.
Mechanism: Meditation has been linked to increased BDNF levels.
Clinical support: Long-term meditation training (9 months) reduced stress hormones and increased hippocampal volume.https://pmc.ncbi.nlm.nih.gov/articles/PMC11591838/
Application for Fatuma: Even brief, daily guided meditation or breathing exercises can help build resilience in her postpartum journey.
- Therapy (e.g., CBT or Task-Shifted Care)
Why it helps: Therapy challenges negative thought patterns and supports new neural pathways.
Kenya-specific model: Research shows non-specialist workers in Kenya can deliver interventions for depression and PTSD, but sustainability needs cross-sector alignment.
Scalability: Integrating mental health into primary care (as envisioned in Kenya’s action plan) can bring these brain-rewiring tools to more people.
- Physical Activity
Why it helps: Aerobic exercise promotes BDNF release, which strengthens neurons. While specific Kenya-based neuroplasticity exercise studies are limited, global evidence strongly supports this.
Contextual fit: In Kenya, recommending culturally relevant movement (e.g., dance, walking) makes this intervention accessible and sustainable.
- Social Connection & Storytelling
Why it helps: Sharing stories in community groups or peer support fosters bonding, engagement, and psychological safety.
Neurobiological basis: Social interaction and narrative work support plasticity via systems like oxytocin and stress regulation.
- Sleep & Nutrition
Sleep: Deep sleep is essential for brain repair and the consolidation of new neural connections.
Nutrition: Foods rich in omega-3s, antioxidants, and healthy fats support neural health and myelination (insulation of neural wires), boosting plasticity.
What We Must Acknowledge: Limitations and Structural Barriers
Time required: Brain rewiring doesn’t happen overnight. Consistency is required over weeks or months.
Severity of illness: People with severe depression, trauma, or other psychiatric disorders may need a combination of medications and behavioral interventions for optimal neural recovery.https://www.mayoclinic.org/diseases-conditions/mental-illness/diagnosis-treatment/drc-20374974
Local research gaps: While global neuroscience offers strong evidence, there are relatively few neuroimaging-based plasticity studies conducted in Kenya. This limits how confidently we can generalize some findings locally.
Systems barriers: Scaling neuroplasticity-based care depends on political will, trained community workers, funding, and sustained mental-health infrastructure — areas where Kenya is making progress but still faces major hurdles.
A Cultural Grounded Path To Healing
A New Hope for Healing — Rooted in Science and Community. In the clinic, Dr. Mwangi suggests a practical, culturally sensitive care plan for Fatuma:
- A 5–10 minute guided meditation each morning
- A weekly walking group for mothers in her neighbourhood
- Access to a peer-support circle where she can tell and reframe her story
Over a few months, the changes begin to register: Fatuma sleeps better, her mood lifts in small, steady increments, and the fog in her mind slowly clears. These are not miracles — they are the product of intentional rewiring, backed by science.
This is more than hope. It’s neurobiology, aligned with Kenya’s reality, strengthened by community, and powered by the resilience of women like Fatuma.






Leave a comment