Imagine a world where malaria, the mosquito-borne killer that claims over 600,000 lives each year, finally loses its grip. This disease affects mostly children under five. For decades, we’ve armed ourselves with bed nets, sprays, and life-saving drugs. But here’s the twist: what if the real weapon isn’t in the field, but in the lab? Or better yet, in your pocket? Enter quantitative diagnostics—the unsung heroes turning the tide from mere survival to total eradication.
Detection Is Just the Start: Unlock the Secrets of Parasite Load
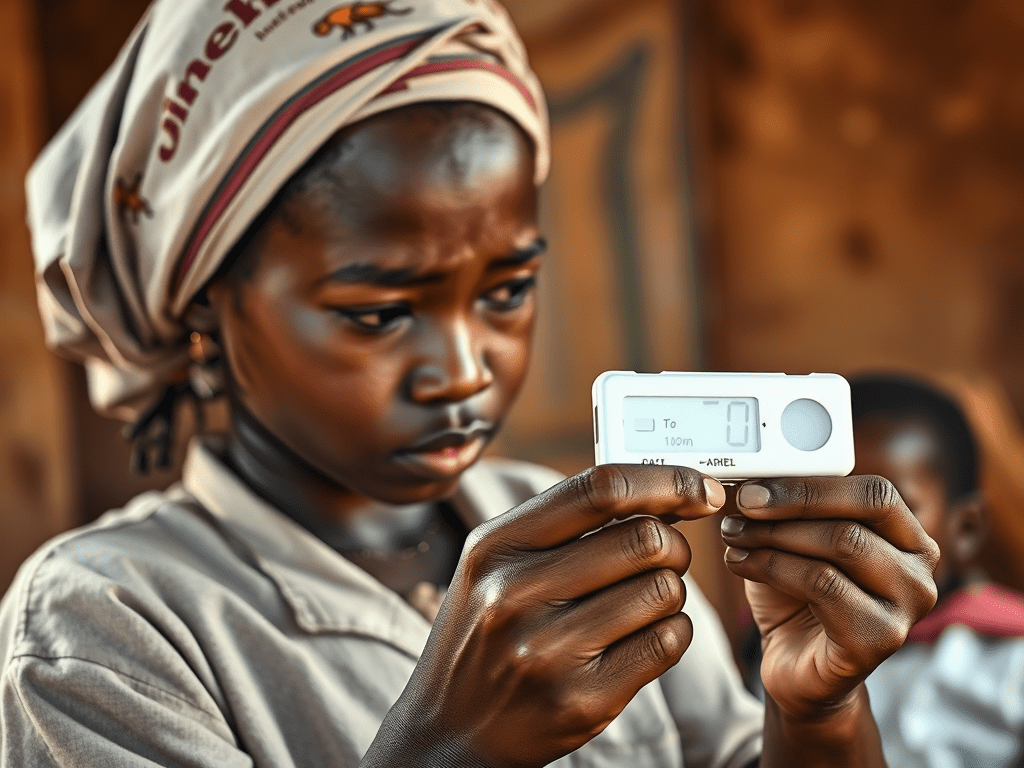
Picture this: A rural clinic in sub-Saharan Africa. A child tests positive for malaria using a simple rapid diagnostic test (RDT). It is a strip of paper that detects the parasite’s fingerprints in the blood. Great news? Sort of. But RDTs and traditional microscopes only answer one question: “Is it there?” They miss the how much. This refers to the parasite density or load. It can range from a whisper. This means a few parasites per microliter of blood. It can also range to a roar. This means hundreds of thousands.
Why obsess over numbers? Parasite load isn’t abstract math; it’s a roadmap to smarter medicine. High loads signal severe illness, demanding aggressive treatment to prevent organ failure. Low loads? They might hide in “asymptomatic carriers”—silent spreaders fueling 20-50% of transmissions in endemic areas. By quantifying, we decode disease severity. We spot drug resistance, like the creeping tolerance to artemisinin drugs. We track how well treatments work. We can even predict outbreaks. It’s like upgrading from a blurry photo to a high-def zoom-in on the enemy.
High Stakes in a Shifting Battlefield
Malaria isn’t standing still—it’s evolving. Climate change is redrawing mosquito maps, pushing the disease into new frontiers like the highlands of Ethiopia. Human migration carries it across borders, while urban sprawl creates perfect breeding grounds in forgotten puddles. Add in parasite mutations and bug-proof mosquitoes, and our old playbook feels outdated.
Enter quantitative diagnostics as our compass. They empower health teams to:
- Hunt the invisible: Pinpoint asymptomatic carriers who feel fine but infect dozens through bites.
- Measure victory: Verify if a drug course wiped out parasites. Check if it just hit pause. This distinction is crucial as resistance rises in Southeast Asia and Africa.
- Sound the alarm: Catch resistance signals early, like a dip in treatment success rates, before it spirals.
- Strike smart: Deploy resources to “hotspots” where loads are sky-high, maximising bang for every donor buck.
Without this precision, we’re swinging in the dark. With it? We adapt, outmanoeuvre, and win.
Tech Revolution: Lab Power in the Palm of Your Hand
The good news? Science is sprinting to catch up. Gone are the days of bulky lab machines. Today’s innovations are rugged, affordable, and field-ready:
- Portable qPCR devices: These are like mini-DNA photocopiers. They amplify and count parasites in under an hour. Their accuracy is within 10 parasites per microliter, rivalling hospital labs.
- AI-boosted digital microscopes: Smartphone attachments scan blood smears. They use machine learning to tally parasites faster than any human eye. The accuracy is 95%.
- Microfluidic biosensors: Tiny chips that sip a blood drop and spit out load data via Bluetooth—perfect for remote villages.
These aren’t gadgets; they’re data engines. In Kenya’s pilot programs, they’ve mapped infection “heat maps,” forecasting flares weeks ahead. In India, they’ve slashed overtreatment by 30%, saving drugs and lives. Suddenly, frontline workers aren’t just reacting—they’re strategising like generals with real-time intel.
Data to Decisions: Fueling the Eradication Engine
Here’s the magic: You can’t fix—or end—what you can’t measure. Quantitative diagnostics flood the system with metrics: infection trends, resistance hotspots, and intervention ROI. Policymakers get dashboards showing if net distribution curbs loads by 40%. Funders see proof that $1 in diagnostics averts $10 in hospital stays. Researchers? They mine the data for breakthroughs, like vaccines targeting high-load strains.
This shifts malaria from gut-feel guesswork to evidence-based mastery. In places like Rwanda, cases have dropped 90% since 2000. Quantitative tools are the next leap. They turn surveillance into a predictive powerhouse.
The Bottom Line: Quantification Isn’t Optional—It’s Our Edge
Killing mosquitoes and popping pills? Vital. But without knowing the scale of the threat, we’re fighting blind. Quantitative diagnostics hands us the clarity to see every parasite, every risk, every win. They make the impossible—malaria’s total defeat—feel within reach.
The fight doesn’t end at “yes or no.” It ignites with “how many?” Let’s count our way to zero.






Leave a comment